State Spends $64M on Health Insurance Web Site
Tuesday, November 27, 2012
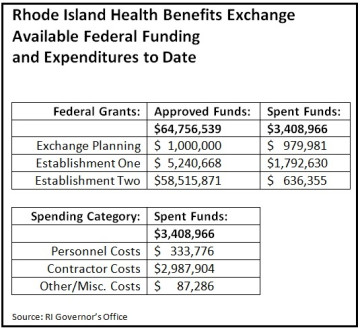
Rhode Island expects to spend $64.7 million on developing and launching its new health benefits exchange, according to state records obtained by GoLocalProv. The exchange—a key piece of the national health reform law passed two years ago—is essentially an online portal where the uninsured will obtain federally subsidized health insurance or enroll in Medicaid.
For now, the cost of launching that portal is being shouldered by three federal grants, but the money will be exhausted by the end of 2014.
After that, the cost of running the exchange will shift to the state—something that has fiscal watchdogs worried.
GET THE LATEST BREAKING NEWS HERE -- SIGN UP FOR GOLOCAL FREE DAILY EBLASTFederal funds run out in by 2015
“The maintenance of the Web site has got to be extremely expensive on an ongoing basis,” said Mark Zaccaria, chairman of the Rhode Island GOP.
He cited estimates that just running the exchanges could cost states upwards of $100 million each.
Rhode Island is one of just 18 states that have chosen to develop their own exchanges.
The rest have opted out and their residents will instead be covered by a nationwide exchange maintained by federal authorities. The cost of Rhode Island’s exchange is less than states like California and New York, each of which is spending $236 million and $183 million, respectively, on developing their exchanges, but those states also have populations many times larger than Rhode Island’s.
Other, smaller-size states, however, are doing theirs for far less than Rhode Island. The exchanges in Iowa and New Mexico are roughly half the cost. Delaware’s is coming in at $4.4 million.
‘Online portal’ costs $64.7 million
The $64.7 million figure covers all of the costs associated with launching the exchange in Rhode Island. The bulk of that is expected to be technology-related expenses, which involve more than just the software and hardware costs associated with the Web site itself.
In order for a successful launch, the exchange will have to update the eligibility system the state uses for Medicaid today. It will also have to sync up with other databases, such as IRS income records, which are key to determining the eligibility of a person seeking a federal subsidy.
The update to the Medicaid system is something the state apparently has been unable to do on its own due to the immense cost involved, according to Linda Katz, the policy director at the Economic Progress Institute and one of a dozen exchange advisory board members.
“Having the money to do this is wonderful because it will streamline coverage for low-income Rhode Islanders,” Katz said.
State officials and other experts yesterday repeatedly emphasized that the exchange is more than “just a Web site.”
“The Exchange is more than a Web site,” said John Cucco, a senior policy analyst at the exchange. “The Exchange is a way for small employers and their employees and individuals … to have an advocate, negotiator, and quality monitor to represent them in their interactions with health insurers and health care providers. The Exchange will also determine eligibility for federal subsidies. Additionally, the Exchange will help people navigate their health insurance and health care questions.”
Additional costs related to the online portal include the following: a customer call center that will field questions from users, an education and outreach program, developing a process for handling appeals and complaints, and managing state and federal requirements.
“The Affordable Care Act (ACA) is a complex law, and implementing it requires a great deal of state-specific work beyond just Web site development,” Cucco said. “[That] includes following new federal regulations, creating changes in Rhode Island’s health care system designed to reduce costs for employers and individuals, and aligning the new program with existing state programs and resources.”
A detailed breakdown of just how much is going to technology or other areas was not available as of press time—and likely won’t be really known for weeks or longer, until the state has completed its negotiations with a private vendor for the work.
“I don’t know that anyone at this point could tell what that dollar amount is,” said Christine Hunsinger, spokesperson for Gov. Chafee, whose office is overseeing the exchange.
Katz said the exchange will benefit all Rhode Islanders by serving as a “one-stop shopping” place online that will provide high-quality health insurance that is affordable, controlling costs and improving care.
Critics question whether site will even work
But some people wonder whether it will even work when it is scheduled to go live on January 1, 2014 (enrollment will actually begin on October 1, 2013).
“Any amount of money is too much because it’s not going to work,” Zaccaria said.
He doubts it will work because of the sheer volume of customers it has to handle. Nationally, an estimated 60 percent of Americans will be using either a state exchange or the federal one. He said the exchanges will have the same level of complexity but many times over the number of users as the stock market. Simply put, nothing on this large of a scale has ever been created, he said.
While the average American may not be using the exchanges on a daily basis, he predicts that brokers who represent “blocks of consumers” will be trolling the online portals incessantly, on the lookout for a deal. The amount of traffic, he said, will overwhelm the state and federal systems.
Pressed for details for how this could happen under the current health reform law, Zaccaria said there are enough “gray areas” in the implementation process to make his scenario plausible.
For example, federal authorities have yet to unveil a centralized “data hub” that states will tap into to access vital data from the IRS and Social Security Administration, according to Edmund Haislmaier, a Senior Research Fellow in Health Policy Studies, at the Heritage Foundation.
What’s driving the cost?
Haislmaier, who helped develop the idea of exchanges in the early 2000s, said the original idea was a far simpler one than the version in the health reform law. In the beginning, he said the exchange would have allowed small businesses to buy defined contribution health insurance plans for their employees. The exchange would have simplified the process for businesses in the sense of being that one-stop shopping place and it also would have allowed them to procure individualized plans for their employees.
“The cost of doing that is relatively small,” Haislmaier said.
Two states adopted exchanges based on his model, according to Haislmaier: Utah and Massachusetts. The exchanges in both states, each with larger populations, cost less than Rhode Island. Massachusetts launched its exchange with an upfront appropriation of $25 million and a staff of 45. Utah got started with just $600,000 and two employees.
But the exchanges established through the health reform law are much more complicated and fundamentally different than the ones he originally envisioned, Haislmaier said.
The Obama-version of the exchanges must have a more robust administrative and technological infrastructure necessary to offer a standardized health insurance package, institute new regulations over and above what each state already has, and create an entirely new subsidy system independent of any that exist today. Plus, the exchange must be able to calculate eligibility for that new subsidy, as well as eligibility for Medicaid and other public programs, according to Haislmaier.
“This is a much bigger task,” Haislmaier said.
The exchanges also have to be able to issue fines to employers who fail to offer health insurance to their workers and calculate payment plans for the uninsured who qualify for only a partial subsidy.
“It goes on and on and on,” said Grace-Marie Turner, the president of the Galen Institute, which promotes “free-market” approaches to health reform.
“States have realized this is going to be hugely costly,” Turner added. “This is an ongoing expense. It’s not a one-time thing. It’s like any bureaucracy.”
Haislmaier also echoed concerns raised by Zaccaria about the sheer volume of users. About 20 percent of households have incomes below 138 percent of the federal poverty level, making them eligible for Medicaid under the expanded criteria of the health reform law. Another 40 percent of households that fall within 138 percent to 400 percent of the poverty level could receive some kind of a subsidy.
All told, that means about 60 percent, or nearly 200 million Americans could be using the exchanges. “You’re looking at an enormous number of people,” Haislmaier said.
If you valued this article, please LIKE GoLocalProv.com on Facebook by clicking HERE.
Related Articles
- Donna Perry: Heated Days for Health Care and Pay Raises
- NEW: Lt. Gov. Roberts Aims to Raise Awareness of Health Care Tax Credits
- Retiree Health Care: Rhode Island’s Other Time Bomb
- EXCLUSIVE: Abortion Fight Threatens Health Care Reform
- NEW: RI Health Care Pros Named to National Advisory Program
- Rob Horowitz: The Politics Rule Out Single-Payer Health Care System
- Harvard Pilgrim Health Care & Tufts Health Plan: Merging?
- NEW: Robert Wood Johnson Foundation to Help RI with Health Care
- State Senate Approves Health Care ‘Exchanges’
- Health Care Costs Skyrocket Since 2010
- NEW: Senator Wants to End Free Health Care for Lawmakers
- Tom Sgouros: Health Care Costs are the Real Crisis
- BREAKING: Pawtucket School Workers Win War on Health Care Retirement Breach
- Health Care Reform: The Five Biggest Questions Facing RI
- NEW: Whitehouse Releases Report on Progress of Health Care Delivery System Reform
- Tufts Health Plan Convenes Quality Forum of Rhode Island Health Care Leaders
- Chafee Officially Establishes Health Care Commission
- Lawmaker Challenges Health Care Exchange Executive Order
- New Health Care Law: How It Will Help RI Children
- Chafee Picks Roberts for Health Care Task Force
- NEW: Delegation to Discuss Health Care Innovation in RI
- Cicilline Announces Federal Help for Dell Health Care Employees
- NEW: Langevin Pushes for Job Creation in Health Care Fields
- Patient Centered Medical Homes: A Health Care Revolution Worth Supporting